Eosinophilic Esophagitis
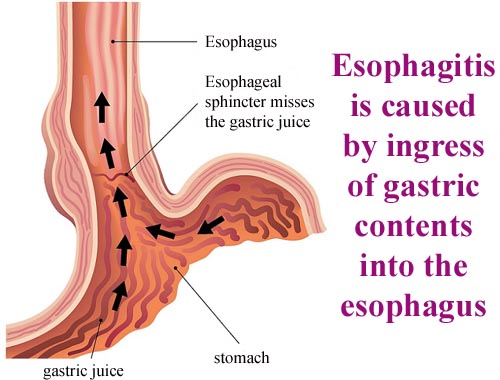
In eosinophilic esophagitis, a type of white blood cell (eosinophil) builds up in the tube that connects your mouth to your stomach (esophagus) as a reaction to foods, allergens or acid reflux. When that happens, the eosinophils can inflame or injure the esophageal tissue. Esophagitis is inflammation that damages tissues of the esophagus, the muscular tube that delivers food from your mouth to your stomach. It is often causes painful, difficult swallowing and chest pain. Causes of esophagitis include stomach acids backing up into the esophagus, infection, oral medications and allergies. Treatments for esophagitis depend on the underlying cause and the severity of tissue damage. If left untreated, esophagitis may change the structure and function of the esophagus. Many of the symptoms experienced by people with GERD and eosinophilic esophagitis overlap. While the symptoms are similar, the treatments are different. The shared symptoms between GERD and eosinophilic esophagitis: nausea; vomiting; abdominal pain; chest pain; difficulty sleeping; The differences between GERD and eosinophilic esophagitis become apparent by looking at the etiology (cause or origin) of the disorders. While GERD is associated with a reflux problem, the cause is unknown in eosinophilic esophagitis. Research, however, shows that allergies and immune system responses are possible causes of eosinophilic esophagitis. Both GERD and eosinophilic esophagitis have involvement of eosinophils in the esophagus. The difference can't really be diagnosed until a biopsy is performed. A small amount of tissue from the esophagus is taken during a procedure called an EGD. Using a high-powered field on a microscope, a count of 15 eosinophils throughout the esophagus is consistent with eosinophilic esophagitis. A count of less than 10 eosinophils at the distal (lower portion) of the esophagus is consistent with GERD.